In medicine, there is a group of diseases referred to as idiopathic, meaning their exact cause remains unknown. Despite numerous studies, doctors are unable to clearly determine what triggers these conditions. One such idiopathic disorder is Irritable Bowel Syndrome (IBS), also known as a sensitive or irritable bowel condition. IBS is a chronic functional gastrointestinal disorder, which means it results from the abnormal functioning of organs rather than structural damage. Although it affects about 25% of the population, its causes are still not fully understood. Irritable Bowel Syndrome (IBS) is characterized by persistent discomfort, abdominal pain and disturbances in bowel habits, such as diarrhoea, constipation, or alternating between the two. The condition is particularly prevalent among young women, who are 2 to 3 times more likely to develop it than men.
Authors: Klaudia Buczek, MSc Eng., and Michał Miśta, MSc Pharm.
Contents:
- Irritable Bowel Syndrome (IBS) – What You Need to Know
- What Are the Causes of IBS?
- Common Symptoms of Irritable Bowel Syndrome (IBS)
- Diagnosing IBS – Rome IV Criteria
- Subtypes of Irritable Bowel Syndrome (IBS)
- How Is Irritable Bowel Syndrome Treated?
- Low FODMAP Elimination Diet
- Sample Meal Plan Incorporating Low FODMAP Foods
- Supplementation in IBS
- Conditions Coexisting with IBS
- Conclusion
- References
1. Irritable Bowel Syndrome (IBS) – What You Need to Know
rritable Bowel Syndrome (IBS) is one of the most commonly diagnosed gastrointestinal disorders worldwide. It is estimated to affect 7 to 15% of the global population, making it a significant health issue for both patients and healthcare systems. While IBS is not associated with severe intestinal damage or an increased risk of developing cancer, its symptoms can significantly reduce the quality of life. People suffering from IBS often face difficulties in daily functioning, including a lowered mood, anxiety, and even depression resulting from the distressing symptoms and psychological disturbances related to IBS.
Although IBS is a functional, not an organic disorder, its impact on patients’ daily lives can be substantial. Therefore, early diagnosis and appropriate therapeutic measures are crucial. Proper management of IBS, including the implementation of a low FODMAP diet, can not only reduce the severity of symptoms but also improve the overall health and quality of life of patients.
The low FODMAP protocol, often used in the diet for IBS, is particularly recommended as it helps alleviate symptoms by eliminating foods that may exacerbate them. Malabsorption disorders and disturbances in the gut microbiota also play a significant role in IBS; therefore, a personalized diet that considers individual intolerances and patient preferences can provide considerable benefits.
2. What are the causes of IBS?
IBS is a complex condition with causes that are not fully understood, but it is known that multiple factors and pathophysiological mechanisms contribute to its development. One of the key mechanisms is a disturbance in gastrointestinal motility. In people with IBS, the intestines may exhibit abnormal movement, leading to abdominal pain, diarrhoea, or constipation. In some patients, the intestines react too strongly to normal stimuli, causing excessive intestinal muscle contractions.
Disturbances in the perception of stimuli are another important factor. In people with IBS, there may be hypersensitivity to the stretching of the intestines, causing discomfort or pain during normal digestive processes that would not trigger these sensations in healthy individuals.
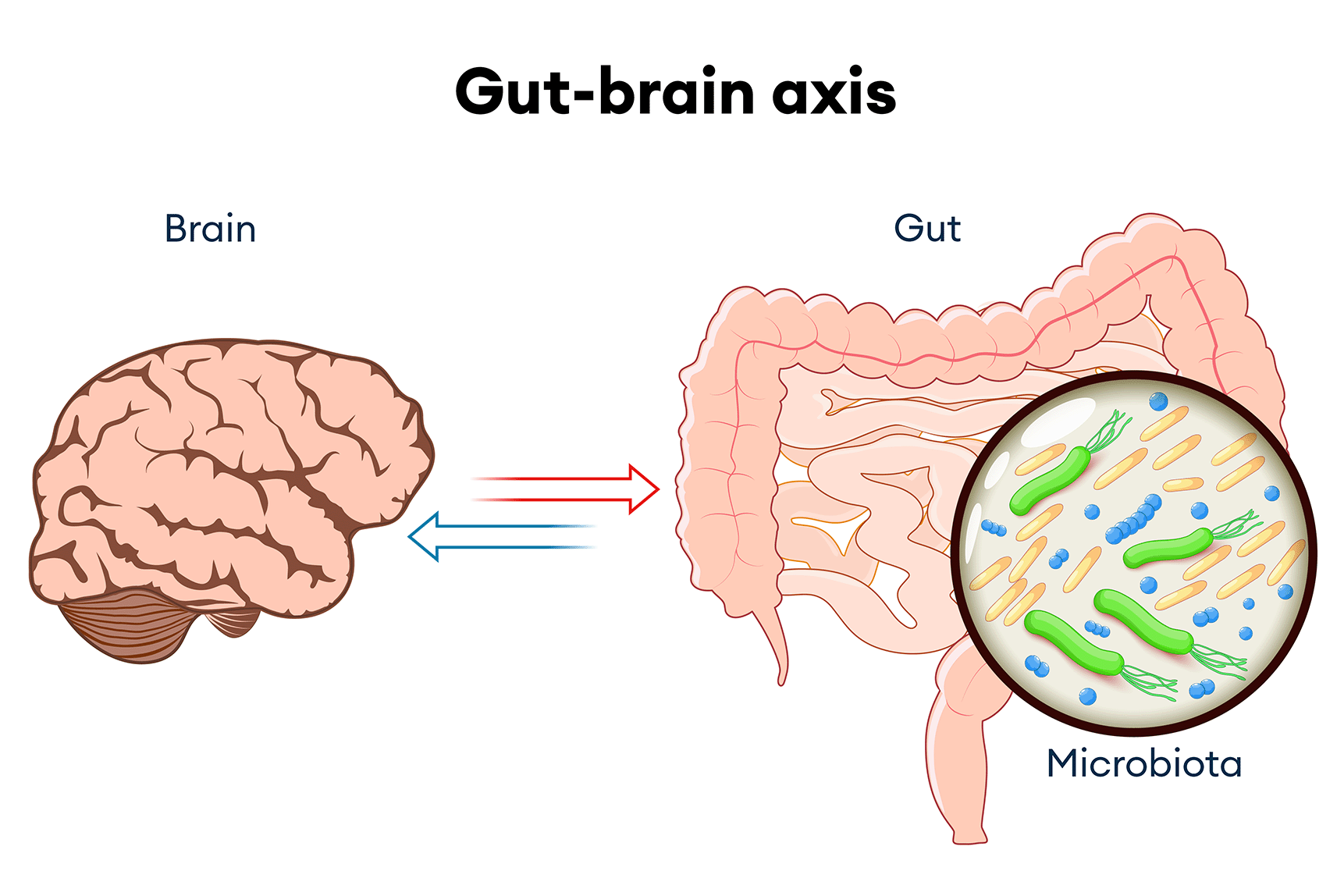
Hormonal and neuropsychological disturbances play a significant role in the onset of irritable bowel syndrome. Stress hormones, such as cortisol, can affect intestinal function, as can changes in the balance of neurotransmitters in the brain responsible for regulating the digestive tract. These disturbances are closely linked to the gut-brain axis, which plays a key role in regulating the interactions between the intestines and the nervous system.
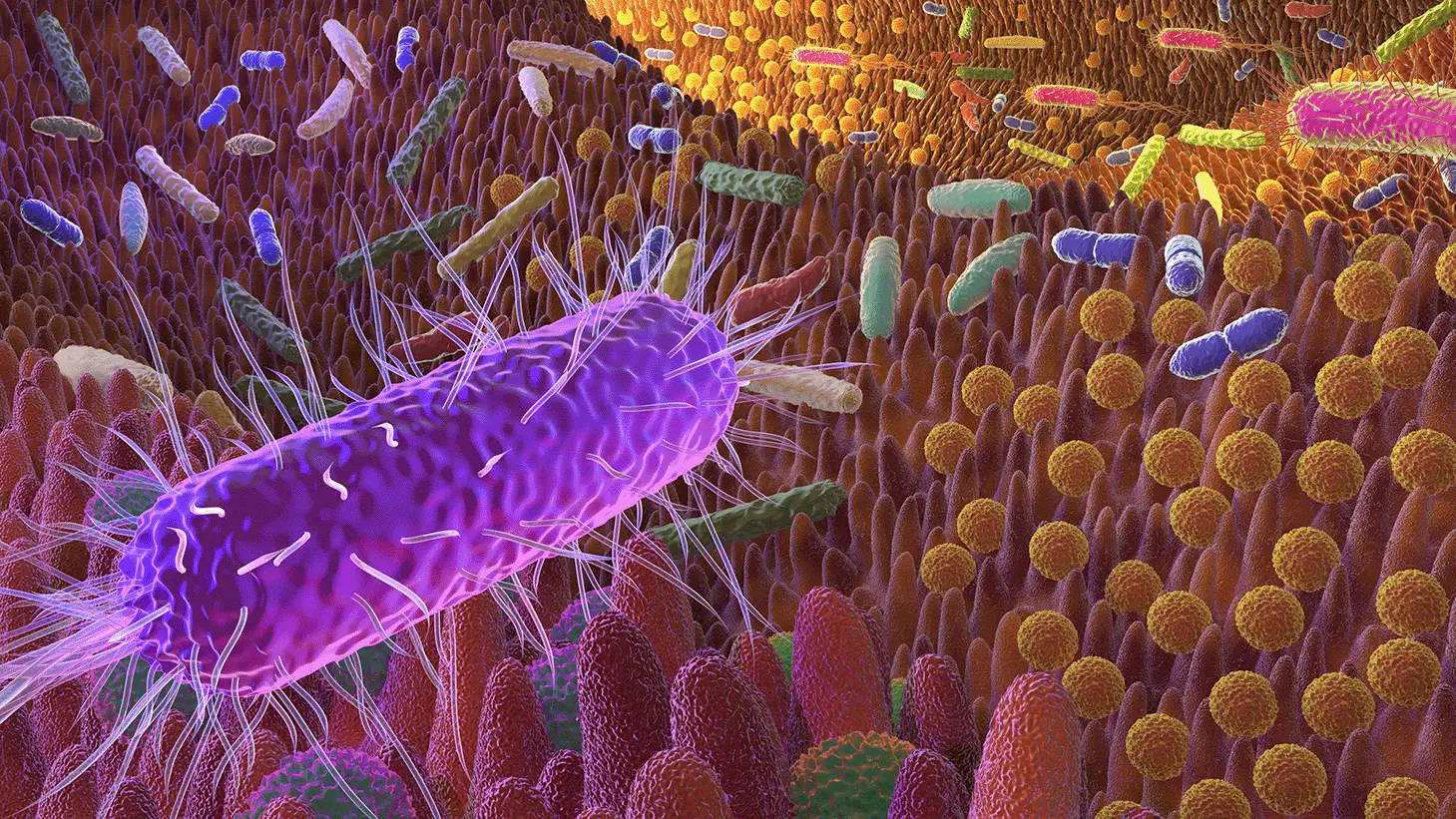
Disturbances in the gut microbiome, or changes in the natural balance of bacteria in the intestines, may contribute to the development of irritable bowel syndrome. Small Intestinal Bacterial Overgrowth (SIBO), a condition where an excessive number of bacteria grows in the small intestine, can affect digestion and cause IBS symptoms such as bloating, abdominal pain, and irregular bowel movements.
Nutritional deficiencies, particularly a lack of fiber in the diet, are also associated with IBS. Fiber plays a key role in the proper functioning of the intestines, and its deficiency can lead to digestive disorders and exacerbate IBS symptoms.
Finally, past intestinal infections can lead to inflammation of the gut and the development of post-infectious IBS. In some individuals, IBS develops after gastrointestinal infections, which may cause lasting changes in bowel function, leading to chronic symptoms.
As seen, Irritable Bowel Syndrome (IBS) is a condition with a complex origin, involving multiple factors and mechanisms that contribute to its development. Intestinal motility disorders, hormonal and neuropsychological disturbances, disruptions in the gut-brain axis, microbiome imbalances, and nutritional deficiencies, such as a lack of fiber, can all contribute to the onset and exacerbation of IBS symptoms. Early recognition and understanding of these mechanisms are crucial for effectively managing this condition.
Photo 1. The gut-brain axis is a complex system of bidirectional communication between the brain and the gastrointestinal tract. It influences the functioning of both the digestive system and the central nervous system, playing a key role in regulating digestion, mood, and the response to stress. Disruptions in the gut-brain axis may contribute to the development of conditions such as Irritable Bowel Syndrome (IBS), where abnormal communication between the gut and the brain leads to the worsening of symptoms. Understanding this complex interaction is essential for a holistic approach to treating IBS.
3. Common Symptoms of Irritable Bowel Syndrome (IBS)
Irritable Bowel Syndrome (IBS) is a chronic condition that affects the functioning of the digestive tract, leading to a range of distressing symptoms. The symptoms of IBS are varied and can include both physical discomfort and psychosomatic disturbances. The most characteristic symptoms of IBS include:
- Abdominal pain and discomfort: This is the most typical symptom of IBS, often worsening after meals and decreasing after a bowel movement. The pain may be experienced as cramping, stabbing, or a feeling of fullness in the abdomen.
- Altered bowel habits: IBS leads to significant digestive disturbances, which can manifest as chronic constipation, diarrhoea, or alternating between the two. Some patients primarily experience constipation (IBS-C), others predominantly diarrhoea (IBS-D), while some have alternating symptoms (IBS-M).
- Bloating and gas: Abdominal bloating and excessive gas are common symptoms of IBS, which may worsen throughout the day, especially after consuming meals high in fermentable carbohydrates (FODMAPs).
- Incomplete evacuation: Patients often feel that their bowels do not empty completely, leading to additional discomfort and a need for more frequent bathroom visits.
- Changes in stool consistency: Stools may range from hard and lumpy to loose or watery, reflecting the variability of IBS symptoms.
The gut microbiome plays a crucial role in the development and manifestation of IBS. Research suggests that dysbiosis, or an imbalance in gut bacteria, may be one of the factors contributing to the worsening of IBS symptoms. Additionally, psychosomatic disturbances, such as stress, anxiety, or depression, can influence IBS symptoms and exacerbate the condition.
Understanding the symptoms of IBS is crucial for effectively managing the condition. This knowledge allows patients to better control their symptoms by making appropriate dietary changes, adjusting their lifestyle, and taking steps to improve their mental well-being.
Photo 2. The gut microbiota consists of approximately 10^14 microbial residents within the human body, far outnumbering the host’s cells! As a result, the number of microbiota genes is at least 100 times greater than the number of human genes, creating a unique ecosystem crucial for health and bodily balance. The bacterial flora in the gut is unique to each individual, and its balance is essential for health but can be easily disrupted during illness. This is particularly significant in the case of Irritable Bowel Syndrome (IBS). It is important to remember that the microbiota (the collection of microorganisms) differs from the microbiome (their genome), and a personalized diet can help support this delicate balance, alleviating IBS symptoms.
4. Diagnosing IBS – Rome IV Criteria
The diagnosis of Irritable Bowel Syndrome (IBS) is based on the so-called Rome Criteria. This name originates from the location of the first international conference on functional gastrointestinal disorders held in 1988 in Rome. During this conference, specialists from around the world developed the first set of guidelines, which became the foundation for subsequent editions of the criteria, such as I, II, and III. The currently applicable Rome IV Criteria serve as a set of international guidelines for diagnosing functional gastrointestinal disorders.
According to these criteria, IBS is diagnosed based on the presence of abdominal pain for at least one day per week over the past three months, associated with at least two of the following factors:
- Pain related to defecation: Abdominal pain or discomfort occurs in connection with bowel movements.
- Change in stool frequency: A significant change in the frequency of bowel movements, manifesting as either diarrhea or constipation.
- Change in stool consistency: A change in the shape or consistency of the stool, which may range from hard and lumpy to loose and watery.
It is important to emphasize that an IBS diagnosis should only be made by a doctor, who can rule out other possible causes of symptoms, such as inflammatory bowel diseases, celiac disease, or gastrointestinal cancers. The doctor may also order additional tests, such as blood tests, food intolerance tests, or a colonoscopy, to ensure that the patient’s symptoms truly meet the criteria for IBS.
IBS is a condition that requires a holistic approach, and a diagnosis based on the Rome IV Criteria is the first step in developing an effective treatment plan. Therapy often involves dietary changes, pharmacotherapy, and psychological interventions to effectively manage symptoms and improve the patient’s quality of life. It is important to remember that an IBS diagnosis is based on ruling out other potentially causative conditions, such as inflammatory bowel disease, making consultation with a doctor essential.
5. Subtypes of Irritable Bowel Syndrome (IBS)
Depending on the predominant symptoms, IBS is divided into four main subtypes: IBS-C, IBS-D, IBS-M, and IBS-U. Each of these subtypes is characterized by a different symptom pattern, which is crucial for the diagnosis and treatment of patients.
IBS-C (IBS with Constipation)
IBS-C, or Irritable Bowel Syndrome with Constipation, is a subtype characterized by predominantly hard or lumpy stools. Individuals with IBS-C experience constipation that can be painful and cause a feeling of incomplete evacuation. In addition to bowel movement difficulties, patients often report abdominal pain, bloating, and discomfort, which can significantly reduce their quality of life. Understanding the mechanisms underlying IBS-C is crucial for implementing effective dietary interventions that can help regulate bowel movements and alleviate symptoms.
IBS-D (IBS with Diarrhea)
In the case of IBS-D, or Irritable Bowel Syndrome with Diarrhoea, the main issue is frequent, loose, or watery stools. Individuals with this subtype often experience a sudden and urgent need to use the restroom, which can be particularly disruptive to daily life. IBS-D may be associated with excessive intestinal motility and an abnormal response to stress. Treating this subtype requires understanding the triggering factors and implementing an appropriate diet that can help alleviate diarrhoea symptoms.
IBS-M (Mixed IBS)
IBS-M, or Mixed Irritable Bowel Syndrome, is characterized by alternating periods of constipation and diarrhoea. Patients with this subtype may experience both hard and loose stools within a short period. This variability in symptoms can be particularly frustrating and challenging to manage. In IBS-M, it is important to monitor diet and lifestyle to identify patterns and potential triggers that may worsen symptoms.
IBS-U (Unclassified IBS)
IBS-U, or Unclassified Irritable Bowel Syndrome, is a subtype in which the symptoms do not clearly fit into any of the above categories. Individuals with IBS-U may experience variable and nonspecific symptoms that are not distinct enough to be classified as IBS-C, IBS-D, or IBS-M. This subtype can be challenging to diagnose and treat, as it requires a personalized approach for each patient.
6. How Is Irritable Bowel Syndrome Treated?
The treatment of IBS requires a comprehensive approach and often involves collaboration among several specialists, such as a dietitian, gastroenterologist, and, in some cases, a psychologist or psychiatrist. An individualized approach is essential, as IBS symptoms can vary greatly from person to person.
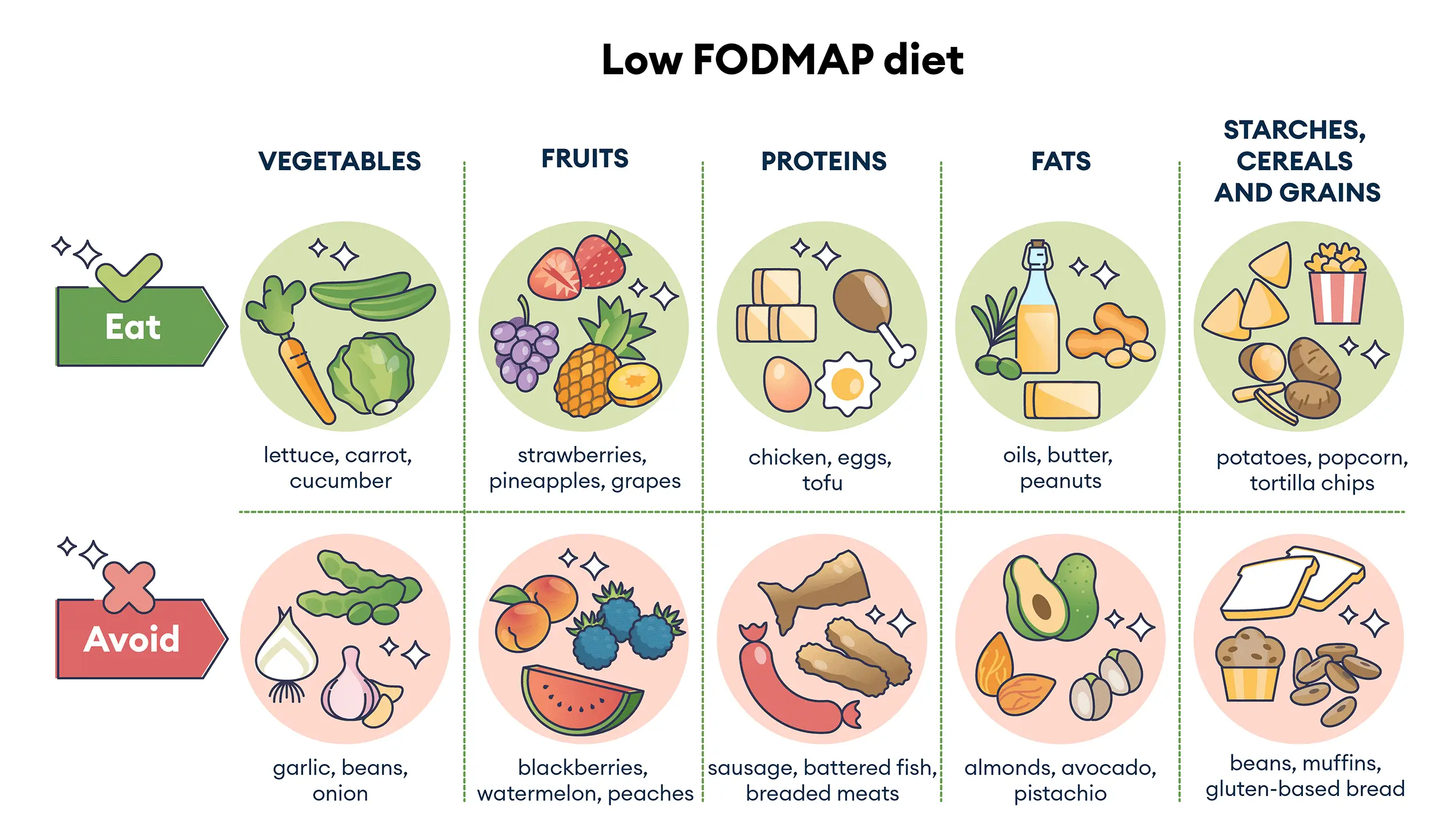
- Diet: Dietary therapy is the cornerstone of IBS treatment. In many cases, the use of a low FODMAP diet is recommended to help alleviate symptoms. This diet involves eliminating fermentable oligosaccharides, disaccharides, monosaccharides, and polyols. Low FODMAP foods, such as rice, carrots, cucumber, and meat, are generally well tolerated, while high FODMAP foods, like onions, garlic, wheat, and dairy products, may exacerbate symptoms.
- Supplementation: Supplementation is an important aspect of treatment but should be tailored to individual needs. Useful supplements include probiotics, sodium butyrate, and herbal remedies like Iberogast. Probiotics support a healthy gut microbiota, which can help alleviate IBS symptoms.
- Pharmacotherapy: Medications frequently used in the treatment of IBS include antispasmodics, which help relieve pain and intestinal cramps. If symptoms are related to stress or depression, the doctor may recommend antidepressants to improve mental well-being and alleviate symptoms.
- Psychological support: IBS is strongly linked to psychological factors. Stress, anxiety, and depression can worsen symptoms. Cognitive Behavioral Therapy (CBT) can help patients manage emotions and stress, improving their quality of life. Anxiety disorders related to IBS may involve worries about eating and social situations. Psychosomatic symptoms may manifest through gastrointestinal discomfort. Eating disorders, such as food avoidance, and depression associated with IBS can impact well-being and gut function. Sleep disturbances related to IBS may include difficulty falling asleep. Relaxation techniques, such as meditation and breathing exercises, can help reduce stress and improve sleep quality.
7. Low FODMAP Elimination Diet
The Low FODMAP diet is a highly recommended nutritional approach for managing Irritable Bowel Syndrome (IBS). This dietary therapy involves limiting the intake of easily fermentable oligosaccharides, disaccharides, monosaccharides, and polyols, which are collectively referred to as FODMAPs. The low FODMAP protocol is a key component of the diet, helping to identify foods that trigger symptoms and tailor the diet to the patient’s individual needs. Keeping a food diary while following the low FODMAP diet is advised to accurately monitor the body’s reactions to different FODMAP groups and better manage IBS treatment.
Why do FODMAP-containing foods trigger symptoms in IBS patients?
A diet high in FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) can exacerbate the symptoms of Irritable Bowel Syndrome (IBS) due to the specific properties of these compounds. FODMAPs are carbohydrates that are more difficult to digest and absorb. High consumption of FODMAP-rich foods can lead to symptoms such as bloating, abdominal pain, and diarrhea in individuals with visceral hypersensitivity. Below, you will learn how each group of FODMAPs contributes to digestive issues.
Fructose, a monosaccharide and one of the smallest compounds in the FODMAP group, plays a key role in triggering IBS symptoms, especially when consumed in excess relative to glucose. Fructose has a strong osmotic effect, meaning it draws water into the intestinal lumen. This can lead to stretching of the intestinal walls, increased pressure, and consequently, bloating, abdominal pain, and diarrhoea. Although fructose is typically absorbed in the small intestine, this process can be impaired in 30-40% of the population, particularly when fructose exceeds glucose. Foods like honey, apples, pears, watermelon, and mango contain more fructose than glucose, which can exacerbate IBS symptoms.
Lactose is a disaccharide found in dairy products that must be broken down into glucose and galactose by the enzyme lactase to be properly digested. In individuals with lactase deficiency or absence, lactose is not digested and passes into the large intestine in its unchanged form. Undigested lactose draws water into the intestinal lumen, which can lead to diarrhoea, and is also fermented by gut bacteria, resulting in gas, bloating, and abdominal pain. Milk and dairy products, such as yogurt and milk-based ice cream, are sources of lactose and can exacerbate IBS symptoms, so it is often recommended to limit their consumption or opt for lactose-free alternatives.
Polyols, such as sorbitol and mannitol, are sugars that are incompletely digested in the small intestine by most people. Due to their small molecules, polyols draw water into the intestinal lumen, which can lead to diarrhoea. Additionally, polyols that are not absorbed can be fermented by gut bacteria, resulting in gas buildup, bloating, and abdominal pain. Foods like cauliflower, apples, pears, and mushrooms contain polyols and may exacerbate symptoms of Irritable Bowel Syndrome (IBS).
Oligosaccharides, including fructans and galactooligosaccharides, are longer-chain carbohydrates that are not digested by humans due to the lack of appropriate enzymes. As a result, oligosaccharides pass through the small intestine unchanged and reach the large intestine, where they are fermented by gut bacteria. While these sugars are beneficial for gut health as they serve as a food source for beneficial bacteria, they can trigger symptoms in people with IBS, especially when consumed in larger amounts. The gases produced during the fermentation of oligosaccharides can lead to bloating, abdominal pain, and disrupted gastrointestinal motility. Oligosaccharides are found in foods such as wheat, rye, onions, garlic, and legumes, which need to be limited in the diet of individuals with Irritable Bowel Syndrome (IBS).
Foods containing FODMAPs can therefore exacerbate IBS symptoms due to their ability to draw water into the intestines and undergo fermentation by gut bacteria. Implementing a low FODMAP diet is crucial for managing IBS symptoms and improving patients’ quality of life.
Photo 3. The Low FODMAP diet, recommended for managing IBS symptoms, involves choosing foods low in FODMAPs, such as lettuce, carrots, cucumber, fruits low in fermentable sugars, and healthy sources of protein and fats. It is important to avoid high-FODMAP foods, including garlic, onions, beans, certain fruits like watermelon and peaches, as well as processed meats and gluten-containing products. Following a Low FODMAP diet for IBS helps reduce bloating, abdominal pain, and other discomforts, thereby improving quality of life.
How to Implement a Low FODMAP Diet?
Implementing a low FODMAP diet to manage the symptoms of Irritable Bowel Syndrome (IBS) involves gradually eliminating foods high in fermentable carbohydrates that can exacerbate symptoms. This typical elimination diet, divided into three stages, helps alleviate discomfort, identify problematic food groups, and establish an optimal dietary plan. It is a crucial component in treating IBS, which can significantly improve patients’ quality of life. It is important to remember that the Low FODMAP protocol is not meant to be a lifelong diet and should be followed under the supervision of a dietitian!
Stage 1: Elimination of High FODMAP Foods
In the first stage of the low FODMAP diet, high FODMAP foods are eliminated to help reduce symptoms by limiting the intake of ingredients that are difficult to digest and absorb, and that ferment in the intestines, exacerbating symptoms in people with visceral hypersensitivity. This restrictive elimination phase should last from 2 to 6 weeks. For children, individuals with other dietary restrictions, or those with coexisting conditions where there is a risk of nutritional deficiencies, a less restrictive approach may be advisable, limiting only selected high-FODMAP foods.
Stage 2: Reintroduction of FODMAPs
In the second stage of the low FODMAP diet, the patient gradually reintroduces individual foods from each FODMAP group, starting with small amounts and gradually increasing them. This stage aims to determine which foods are well-tolerated and which trigger IBS symptoms. Patients monitor their reactions not only to specific foods but also to their quantities, allowing for a precise understanding of individual tolerance. Keeping a food diary during this phase is crucial to effectively track the body’s responses to different foods and their portions. The reintroduction stage typically lasts from 6 to 8 weeks.
Stage 3: Personalization of a FODMAP-Restricted Diet
The final stage of the Low FODMAP diet involves implementing an individualized, varied diet based on foods that are well-tolerated. Personalizing the diet to suit your unique needs is crucial for long-term control of IBS symptoms. In this phase, it is important for the diet to be not only diverse but also nutritionally complete, providing all the essential nutrients while helping to prevent symptom flare-ups. This approach enables you to manage your condition more effectively and maintain a sense of well-being.
Effectiveness of the Low FODMAP Diet
Numerous studies have shown that following a Low FODMAP diet can be effective in managing IBS, particularly in reducing symptoms such as bloating, abdominal pain, and diarrhoea. The implementation and adherence to the Low FODMAP protocol should always be supervised by a dietitian, who can guide the patient through all phases of the diet, monitor the body’s responses, and adjust the dietary plan according to individual needs.
The Low FODMAP diet, used in the dietary management of IBS, is a powerful tool; however, it is important to follow it responsibly, with a full understanding of its stages and goals. When correctly implemented, this elimination diet can significantly enhance patients’ quality of life by helping them manage IBS symptoms and enjoy better health.
8. Sample Meal Plan Incorporating Low FODMAP Foods
Irritable Bowel Syndrome (IBS) is a condition that requires special attention when planning a diet. The Low FODMAP diet is an effective approach that can help alleviate IBS symptoms by limiting the intake of easily fermentable oligosaccharides, disaccharides, monosaccharides, and polyols. Here is a sample one-day meal plan that includes low FODMAP foods, perfectly aligning with the principles of the Low FODMAP diet recommended for IBS.
Breakfast
Spinach and Feta Cheese Omelette
- 2 eggs
- 2 handfuls of fresh spinach
- 25 g feta cheese
- 1 teaspoon olive oil
- 1 tablespoon pine nuts
- 2 slices of spelt bread
Mid-Morning Snack
Lactose-Free Yogurt with Blueberries and Pumpkin Seeds
- 150 g lactose-free natural yogurt
- 2 handfuls of fresh blueberries
- 1 tablespoon pumpkin seeds
Lunch
Grilled Chicken Breast with Rice and Salad
- 150 g chicken breast (seasoned with salt, pepper, and herbs)
- 50 g basmati rice
- 1 tablespoon olive oil
- Fresh herbs (e.g., parsley, dill)
Arugula, Carrot, and Cucumber Salad
- 2 handfuls of fresh arugula
- 1 carrot cut into long ribbons
- 1/2 cucumber sliced into half-moons
- 1 tablespoon olive oil
- Salt, pepper, and lemon juice to taste
Afternoon Snack
Orange with Almonds
- 1/2 orange (about 120 g)
- 1 tablespoon almonds
Dinner
Baked Salmon with Potatoes and Green Beans
- 150 g salmon fillet
- 2 medium-sized potatoes
- 75 g green beans
- 1 tablespoon olive oil
- Lemon juice and fresh herbs (e.g., dill) to taste
By following a low FODMAP diet and carefully planning meals, individuals with IBS can effectively manage their symptoms, making the proper implementation of the low FODMAP diet one of the key elements of therapy.
Photo 4. Sanprobi IBS is a popular probiotic containing the Lactiplantibacillus plantarum 299v strain, which supports gut health, particularly in individuals suffering from Irritable Bowel Syndrome (IBS). It works by modulating the gut microbiota, helping to reduce symptoms such as bloating, abdominal pain, and irregular bowel movements. The use of Sanprobi IBS is often recommended as a supplement to the low FODMAP diet in IBS management, which can further enhance the effectiveness of the treatment. Lactiplantibacillus plantarum 299v is one of the most thoroughly researched probiotic strains worldwide, with its effectiveness confirmed in numerous clinical studies.
9. Supplementation in IBS
In the treatment of Irritable Bowel Syndrome (IBS), supplementation can play a key role in alleviating symptoms and supporting gastrointestinal health. In the context of IBS, special attention is given to supplements that support the gut microbiome, which is a crucial factor in maintaining intestinal balance and improving gut function.
Probiotics and Their Role in IBS
Probiotics are supplements containing beneficial bacteria that can support the gut microbiome and, consequently, help alleviate IBS symptoms. Numerous studies indicate the effectiveness of various probiotic strains in improving gastrointestinal function in the context of Irritable Bowel Syndrome.
- Bacillus coagulans is a probiotic strain that is gaining increasing recognition in the treatment of Irritable Bowel Syndrome (IBS). Numerous studies have shown that combining IBS treatment with supplementation of this probiotic can help alleviate symptoms such as abdominal pain, bloating, and irregular bowel movements, including both diarrhea and constipation. Bacillus coagulans works by modulating the gut microbiota, promoting a better balance between beneficial and pathogenic bacteria in the intestines, and supporting the intestinal barrier. Additionally, its ability to survive in the acidic environment of the stomach and its high stability in supplement form make it effective in reaching the intestines and exerting a positive effect. Regular use of Bacillus coagulans can significantly improve the quality of life for patients with IBS by reducing the severity of symptoms and enhancing overall gastrointestinal function.
- Lactiplantibacillus plantarum 299v – This bacterial strain is particularly effective in reducing symptoms such as bloating and abdominal pain. Studies show that regular use of this probiotic can significantly improve the quality of life for IBS patients. It is an ingredient in the popular product Sanprobi IBS, a probiotic particularly recommended for IBS patients, as it contains a combination of strains that can help regulate the gut microbiome. Regular use of Sanprobi IBS may help reduce bloating, abdominal pain, and improve bowel movement regularity.
- Lactobacillus rhamnosus GG: This is one of the most well-researched probiotic strains, known for its beneficial effects on the gastrointestinal tract. Supplementation with this strain can help restore the gut microbiota, which is crucial for alleviating IBS symptoms.
- Bifidobacterium bifidum: This strain is valued for its gut health-supporting properties. Supplementation with Bifidobacterium bifidum may help improve digestion and reduce symptoms commonly associated with Irritable Bowel Syndrome, such as diarrhea and constipation.
- Saccharomyces boulardii: These probiotic yeasts can be helpful in regulating gastrointestinal function, especially in cases of diarrhea associated with IBS. Supplementation with Saccharomyces boulardii also aids in restoring the natural gut microbiota after antibiotic therapy.
How to Choose Supplements for IBS?
The selection of probiotic supplements should be personalized, taking into account the individual symptoms and needs of the patient. Introducing the right supplements can support gut function, alleviate IBS symptoms, and improve overall quality of life. It is crucial to carry out supplementation under the guidance of a specialist who can help choose the appropriate products and monitor their effects.
In the case of Irritable Bowel Syndrome, the gut microbiome plays a crucial role in maintaining gastrointestinal health. Regular use of probiotics such as Bacillus coagulans, Lactiplantibacillus plantarum 299v (Sanprobi IBS), Lactobacillus rhamnosus GG, Bifidobacterium bifidum, and Saccharomyces boulardii can help reduce symptoms, improve gut comfort, and restore the natural balance of the gut microbiome.
10. Conditions Coexisting with IBS
Irritable Bowel Syndrome (IBS) is a condition that often coexists with other disorders, both psychological and somatic. These comorbidities can not only exacerbate IBS symptoms but also complicate the treatment process. Below, we discuss the most common conditions that coexist with IBS.
Fibromyalgia
Fibromyalgia is one of the most common conditions coexisting with IBS. It is characterized by chronic, widespread musculoskeletal pain and sensitivity to touch. Both conditions share similar pathophysiological mechanisms, such as altered pain processing in the central nervous system, suggesting they may have a common underlying cause. Patients suffering from fibromyalgia often also report IBS symptoms, which requires an integrated therapeutic approach.
Psychological Disorders Associated with IBS
Psychological disorders are commonly observed in individuals with IBS. Anxiety and depressive disorders related to IBS occur much more frequently than in the general population. Anxiety and depression can both exacerbate IBS symptoms and result from the chronic pain and discomfort associated with the condition. Treating psychological disorders, often using relaxation techniques and psychotherapy, is crucial in the comprehensive management of IBS.
Sleep Disorders Associated with IBS
Sleep disorders are another issue that often affects patients with IBS. Individuals with IBS frequently complain of difficulty falling asleep, frequent nighttime awakenings, and feeling unrefreshed despite seemingly adequate sleep duration. Sleep disturbances can exacerbate IBS symptoms, leading to a vicious cycle where IBS symptoms affect sleep quality, and poor sleep further aggravates gastrointestinal discomfort.
Emotional and Psychosomatic Disorders Associated with IBS
Emotional disorders, such as stress, anxiety, and depression, have a significant impact on the course of IBS. Irritable Bowel Syndrome is often classified as a psychosomatic disorder, where physical symptoms are closely linked to the patient’s emotional state. Therapy focused on improving mental health, including relaxation techniques, can help alleviate IBS symptoms by reducing their severity.
Eating Disorders Associated with IBS
Eating disorders, such as anorexia or bulimia, can occur in individuals with IBS. Unhealthy eating habits, often stemming from attempts to cope with IBS symptoms, can lead to serious health problems. Collaboration with a dietitian and a psychotherapist is essential for effectively managing both IBS and eating disorders.
Psychosocial Disorders Associated with IBS
IBS can also impact a patient’s social life. Chronic pain, discomfort, and fear of sudden symptoms may lead to withdrawal from social activities, which in turn can exacerbate psychological and emotional problems. Psychosocial disorders associated with IBS require not only medical support but also psychological care to help the patient function normally in daily life.
11. Conclusion
Understanding that IBS is an idiopathic condition is key to effectively managing its symptoms. While the lack of a clear cause can be frustrating, there are proven methods that provide relief. A holistic approach, including dietary therapy, plays a crucial role in alleviating discomfort. By eliminating high-fermentable carbohydrate foods and adopting a low-FODMAP diet, symptoms can be significantly reduced while maintaining gut health. Eating disorders related to IBS, such as avoiding food due to fear of symptoms, can further complicate the situation, making a comprehensive treatment approach essential. It is also important to consider the role of the gut-brain axis, which can influence symptom intensity. Therefore, in addition to dietary changes, psychological support and, if necessary, pharmacotherapy may be required. An integrated approach that considers all these aspects provides the best results and helps patients regain control over their lives.
12. References
- Współczesna dietoterapia, Lange Ewa, Włodarek Dariusz, PZWL, Warszawa 2022, https://pzwl.pl/Wspolczesna-dietoterapia,197971021,p.html
- Efficacy of a low FODMAP diet in irritable bowel syndrome: systematic review and network meta-analysis. Black CJ, Staudacher HM, Ford AC. Gut. 2022 Jun;71(6):1117-1126. doi: 10.1136/gutjnl-2021-325214. Epub 2021 Aug 10. PMID: 34376515. https://pubmed.ncbi.nlm.nih.gov/34376515/
- Efficacy of Probiotics for Irritable Bowel Syndrome: A Systematic Review and Network Meta-Analysis. Zhang T, Zhang C, Zhang J, Sun F, Duan L. Front Cell Infect Microbiol. 2022 Apr 1;12:859967. doi: 10.3389/fcimb.2022.859967. PMID: 35433498; PMCID: PMC9010660. https://pubmed.ncbi.nlm.nih.gov/35433498/
- Efficacy of an Irritable Bowel Syndrome Diet in the Treatment of Small Intestinal Bacterial Overgrowth: A Narrative Review, J. P. Wielgosz-Grochowska, N. Domanski, and M. E. Drywień, Nutrients, vol. 14, no. 16, Aug. 2022, doi: 10.3390/NU14163382. https://pubmed.ncbi.nlm.nih.gov/36014888/
- Diet or medication in primary care patients with IBS: the DOMINO study – a randomised trial supported by the Belgian Health Care Knowledge Centre (KCE Trials Programme) and the Rome Foundation Research Institute, F. Carbone et al., Gut, vol. 71, no. 11, pp. 2226–2232, Apr. 2022, doi: 10.1136/GUTJNL-2021-325821. https://pubmed.ncbi.nlm.nih.gov/35483886/
- Health-Related Quality of Life in Irritable Bowel Syndrome: A Systematic Review and Meta-analysis, G. E. Cassar, G. J. Youssef, S. Knowles, R. Moulding, and D. W. Austin, Gastroenterol Nurs, vol. 43, no. 3, pp. E102–E122, May 2020, doi: 10.1097/SGA.0000000000000530. https://pubmed.ncbi.nlm.nih.gov/32487960/
- Controversies and reality of the FODMAP diet for patients with irritable bowel syndrome, E. P. Halmos and P. R. Gibson, J Gastroenterol Hepatol, vol. 34, no. 7, pp. 1134–1142, Jul. 2019, doi: 10.1111/JGH.14650. https://pubmed.ncbi.nlm.nih.gov/30945376/
- Choroby wewnętrzne Davidson. Tom 2, red. wyd. pol. Jacek Różański, Wydawnictwo Edra Urban & Partner, 2018
- Dietoterapia, Dominika Głąbska, Lucyna Kozłowska, Ewa Lange, Dariusz Włodarek, PZWL Wydawnictwo Lekarskie, Warszawa 2014 https://pzwl.pl/Dietoterapia,4930593,p.html
- Podstawy żywienia i dietoterapia, Peckenpaugh Nancy J., Wydawnictwo Medyczne Urban & Partner, Warszawa 2012
- Żywienie Człowieka, Podstawy nauki o żywieniu, tom 2, Redakcja naukowa Jan Gawęcki, Wydawnictwo Naukowe PWN, Warszawa 2012
- IBS and multidisciplinary care, https://www.monashfodmap.com/blog/ibs-and-multidisciplinary-care/, Monash University,
- All about onion, garlic and infused oils on the Low FODMAP Diet…, https://www.monashfodmap.com/blog/all-about-onion-garlic-and-infused-oils-on-the-low-fodmap-diet/”, Monash University
You may also be interested in:
2025-09-30
Energy Slump After Lunch? How Your Diet at Work Improves Concentration and Productivity
What you put on your plate largely determines how you function at the office. Diet and…
2025-03-20
How Diet and Lifestyle Affect Your Immunity?
The immune system is indispensable to our survival. Its primary function is to constantly…
2025-02-24
The Mediterranean Diet – Discover the Principles and Foods of the Healthiest Cuisine in the World!
This diet influences not only physical health but also the way we think about food and…
 PL (PLN)
PL (PLN) EN (GBP)
EN (GBP) EN (EUR)
EN (EUR)